Copyright 2020 Massachusetts Institute of Technology
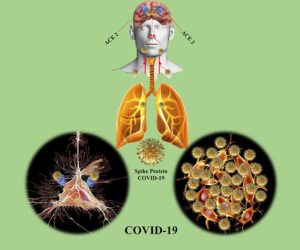
It’s been months since we first felt the effects of the devastating spread of COVID-19. What we know is that the virus often causes a highly infectious viral pneumonia and Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). In addition to the respiratory issues caused by COVID-19, it appears that about one third of all COVID-19 patients also display neurological problems. Does this mean that not only the lungs, but other organ systems, such as the brain and central nervous system, are also affected by this new pathogen?
Yes! COVID-19 can also invade and affect your brain
So how does COVID-19 invade your brain? At first, it seemed that SARS-CoV-2 only targeted the lungs; however, now we know that in order to enter the cells of the lungs, the virus binds to specific ACE2 receptors, a transmembrane protein located in specific vital organs. These receptors seem to allow the virus to move into cells where it multiplies and spreads. The problem is that the ACE2 receptors assist in regulating blood pressure and are not only present in the lungs, but in all vital organs. This makes it possible for SARS-CoV-2 to work its way through the nervous system and reach the brain. Once in the brain, the spread of the virus can cause neurological damage. The science is not clear yet, but this spread may be partially responsible for the respiratory failure that many COVID-19 patients admitted to the Intensive Care Unit (ICU) experience.
The impact of the virus: patients reporting neurological symptoms
We have all heard about the typical symptoms of COVID-19 such as fever, a cough, and shortness of breath. However, it has been reported that some patients also suffer from strokes, seizures, confusion, disorientation, brief loss of consciousness, and brain inflammation. This leads to acute problems in cognitive functions important for participating in daily life.
Copyright 2020 American Chemical Society
These neurological symptoms are sometimes linked to the low oxygen levels in the blood. Clinicians have observed that the virus can have a clotting effect on blood, which means that circulation is hampered and the body, including the brain, does not get enough oxygen. Some scientists think that in addition to blood clotting, the virus may also inhibit the brainstem’s ability to regulate breathing as it normally would. The brainstem is the part of the brain that controls messages between the body and our most basic bodily functions, such as breathing, heart rate, and blood pressure. Scientists believe that due to the effects of COVID-19, the brainstem has difficulties in sensing that the body is not getting enough oxygen. However, in some patients the neurological symptoms appear to be more prominent than the respiratory symptoms; because of this, scientists and doctors are trying to understand which neurological symptoms are caused directly by the virus.
Shockingly, there was a report from Dr. Thomas Oxely, a neurologist at Mount Sinai in New York, who observed something he had never seen before while treating a middle-aged man infected with COVID-19. During the procedure to remove a clot out of a blood vessel in the patient’s brain, the neurologist saw new clots forming around it instantaneously. Before surgery, the man had reported trouble talking and moving the right side of his body, which are common stroke-related symptoms.
Oxely has been working on the front-line due to a shortage of doctors. The patients treated for stroke as a result of the virus were an average of 15 years younger than patients suffering from stroke without COVID-19. “Our report shows a seven-fold increase in incidence of sudden stroke in young patients,” stated Oxely. These young patients without health complication or medical history would typically be classified at very low risk for suffering from a stroke. Thus, it may be important to screen for vascular problems and stroke in post-corona patients of all ages, even in those who only had mild or no COVID-19 symptoms (e.g respiratory problems, coughing/sneezing, and fever), in order to ensure that we limit the repercussions of life threatening conditions and help them get back to their daily lives.
How can telehealth help?

Copyright 2020 The Virtual Reality Company
Now that people all over the world have experienced the difficulties of living under the lockdown conditions of the COVID-19 pandemic, the need for innovative healthcare solutions that allow people to receive remote medical treatment has been highlighted. These solutions are referred to as telehealth or telemedicine. During the height of the crisis, many healthcare systems around the world were forced to be focused exclusively on the overwhelming number of critical COVID-19 patients, while many other important but less urgent treatments had to be postponed.
In our modern society where global travel is a way of life, it is unfortunately inevitable that there will be more of these types of health catastrophes that have far reaching effects. In order to provide the continuous healthcare that is required, telehealth solutions help doctors deliver care even in times of crisis. Telehealth solutions can also be used in cases where the closest medical facilities are far away. In countries with large rural populations, such as the United States, people often have to travel hours to reach the nearest medical facility. NeuroReality’s virtual reality cognitive rehabilitation solution, Koji’s Quest, can be used to provide telerehabilitation to post-stroke and post-Corona patients to retrain cognitive functions which were damaged and promote overall well-being. Koji’s Quest extends the reach of clinicians so that more patients can receive the care they need, not only during these uncertain times, but also when distances prohibit easy access to medical care.
The COVID-19 pandemic has changed our lives for the foreseeable future. Now that we have to sacrifice meeting in-person for the sake of societal health we at NeuroReality believe that digital tools, like Koji’s Quest, can help us all stay connected and healthy.
References
- Brussaard, A. (2020, March 18). SARS‐CoV-2 in COVID-19 patients is likely to infect the brain. Retrieved from https://www.amsterdamresearch.org/web/instituut-1/nieuws/tonenop/sarscov-2-in-covid-19-patients-is-likely-to-infect-the-brain.htm
- Cha, A.E. (2020, April 25). Young and middle-aged people, barely sick with covid-19, are dying of strokes. Retrieved from https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/?fbclid=IwAR0oLeVWk48sKAoWrnVvhoJAh7CDFi3nfg_zm_R9OVQG2b6fDt0zMe8SYW0
- De Jonge, H. (2020, April 29). Helft coronapatiënten op IC heeft stollingen in longen of hersenen. Retrieved from https://nos.nl/nieuwsuur/artikel/2332229-helft-coronapatienten-op-ic-heeft-stollingen-in-longen-of-hersenen.html
- Goodman, B. (2020, April 17). Cytokine Storms May Be Fueling Some COVID Deaths. Retrieved from https://www.webmd.com/lung/news/20200417/cytokine-storms-may-be-fueling-some-covid-deaths
- How COVID-19 Affects the Brain: Confusion, Seizure, Stroke (2020, April 18). Retrieved from https://www.novinite.com/articles/204187/How+COVID-19+Affects+the+Brain%3A+Confusion%2C+Seizure%2C+Stroke
- Topol, E. (2020, March 31). Telemedicine is essential amid the covid-19 crisis and after it. Retrieved from https://amp-economist-com.cdn.ampproject.org/c/s/amp.economist.com/open-future/2020/03/31/telemedicine-is-essential-amid-the-covid-19-crisis-and-after-it
- Wadman, M., Couzin-Frankel, J., Kaiser, J., & Matacic, C. (2020, April 17). How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes. Retrieved from https://www.sciencemag.org/news/2020/04/how-does-coronavirus-kill-clinicians-trace-ferocious-rampage-through-body-brain-toes#